Publisher
India Pharma Outlook
published at
June 11, 2025
Surprise FDA Inspections: Engineering Audit-Readiness into Pharma Facility Design
What if your facility’s next FDA inspection began tomorrow, without warning?
With surprise inspections now the norm across India and other key manufacturing regions, the traditional approach of “just-in-time” audit readiness no longer holds up.
From 2023 to 2025, the U.S. FDA has doubled down on unannounced audits of foreign pharmaceutical sites, driven by persistent GMP lapses, even at facilities given prior notice. Indian sites, in particular, are under intense scrutiny, and many are falling short not due to lack of intent but due to gaps in facility design, validation planning, and operational discipline.
This article is your technical playbook.
We break down how pharma companies can proactively engineer compliance into every layer of facility design- from CQV strategy and cleanroom layout to Annex 1 implementation and supplier control. If you're involved in pharma project management, QA, CQV, or engineering, this guide will show you how to build plants that stand up to the toughest inspections- surprise or not.
The Rise of Surprise FDA Inspections (2023–2025)
In May 2025, the U.S. Food and Drug Administration (FDA) announced a significant policy shift: the expansion of unannounced (surprise) inspections at foreign drug manufacturing sites. This move aims to eliminate the longstanding disparity where U.S. facilities faced no-warning inspections, while many Indian, Chinese, and other foreign manufacturers received advance notice.
This change builds upon a pilot program in India and China and ensures foreign firms receive the same rigorous oversight as domestic ones. The decision was influenced by findings that even with advance notice, FDA inspectors uncovered serious Good Manufacturing Practice (GMP) deficiencies at foreign plants more than twice as often as in U.S. plants.
Implications for Indian Pharma
India, a top supplier of generic drugs, has been a focal point of these unannounced audits. During a 2022–24 FDA pilot, 94 out of 114 inspections in India were unannounced. With about 340 Indian and Chinese drug sites going over five years without FDA inspection due to the pandemic backlog, regulators are now working to get foreign inspections back on track.
Indian facilities should now assume that an FDA investigator could arrive at any time, without warning. This heightened scrutiny means continuous audit readiness is critical, not just ahead of scheduled visits. Firms that delay, obstruct, or deny a surprise inspection face tough enforcement actions, including warning letters, import alerts, or even suspension of product shipments.
The stakes are high for pharma project teams and global QA/QC leaders: audit-readiness can no longer be an afterthought; it must be engineered into the facility and its operations from day one.
Common FDA Inspection Findings and Compliance Pitfalls
Recent FDA Form 483 observations and warning letters reveal recurring GMP lapses that pharma facilities must proactively address. Understanding these top problem areas will help project managers and quality leads "design out" compliance risks:
1. Data Integrity and Recordkeeping Failures
Data integrity remains a cornerstone issue in FDA inspections. In 2024, over 70% of warning letters showed some data integrity component, underscoring persistent problems with incomplete, inaccurate, or falsified records.
Common citations include missing or backdated entries, uncontrolled changes to electronic data, and a lack of audit trails. For example, FDA inspectors in late 2022 caught workers at Intas Pharmaceuticals shredding and hiding quality documents- bags of torn lab records were found under a stairwell and even in a truck outside.
In one egregious case, an analyst was seen pouring acid into a trash bin of test records to destroy evidence. Such incidents led the FDA to criticize Intas for "failing to ensure reliability of data" and poor control of documents and computerized systems.
More broadly, regulators keep citing firms for non-contemporaneous recordkeeping (e.g., not recording test results at the time of performance) and using shared logins or generic user IDs in lab systems- practices that obscure traceability.
Compliance Insight: Quality teams should implement ALCOA+ principles (Attributable, Legible, Contemporaneous, Original, Accurate, etc.) in all data systems. This means designing labs and IT systems so that data entry is time-stamped and locked, original records (paper or electronic) are preserved, and any changes are transparently documented. Robust digital controls (unique user credentials, audit trail software, backup systems) built into the facility’s IT infrastructure are vital.
2. Equipment Qualification and Validation Gaps
Another frequent audit pitfall is inadequate equipment and facility qualification. FDA expects that all manufacturing equipment, utilities, and control systems are fully commissioned and qualified (IQ/OQ/PQ) and kept in a qualified state. Yet in the past two years, many Form 483s highlight lapses such as unqualified devices in use, missing validation documentation, or poor maintenance that compromises sterile conditions.
In one 2024 example, an FDA inspector observed scratches inside an ISO-5 aseptic hood, which meant the surface could not be properly cleaned- a direct contamination risk. Another cited case involved a manufacturer that relocated production equipment without requalification or updated process documents, violating basic change-control and validation protocols.
Even record-keeping around equipment can trip up firms: at a Sun Pharma site, no usage logbooks were kept for QC lab incubators, meaning the company couldn’t track whether critical equipment was cleaned, calibrated, or used appropriately. Such gaps indicate an immature Commissioning, Qualification, and Validation (CQV) program and draw FDA’s ire.
Compliance Insight: Pharma project managers should adopt a "validation-first" mindset during design and construction. That means planning for rigorous commissioning and qualification of each system (process equipment, HVAC, water, etc.) before commercial use, and establishing procedures for re-validation whenever changes occur. Embedding real-time monitoring sensors and alarms can help ensure equipment stays within qualified parameters. Also, maintain detailed equipment files and logs from day one- ideally via an electronic asset management system- so that any inspector can instantly see calibration dates, maintenance, and change history.
3. Contamination Control and Sterility Issues
For facilities making sterile or injectable products, contamination control lapses are among the most critical (and commonly cited) issues. FDA investigators frequently flag poor aseptic techniques, improper cleanroom behaviors, or environmental monitoring deficiencies that could lead to microbial contamination of products.
In early 2023, for instance, FDA inspectors issued a scathing report to Sun Pharma’s Halol plant, citing "a litany of GMP violations, including poor aseptic practices." In another high-profile case (2023), a Cipla manufacturing site in India was written up for eight power failures that shut down HVAC in a supposedly controlled area, as well as hundreds of customer complaints and lab records literally stored in bags of scrap, all pointing to chaotic contamination control and quality oversight.
FDA warning letters in 2023–24 also emphasize failures in environmental monitoring: e.g., not reading incubated microbial plates on time or not investigating environmental excursions. Any such lapse can have direct patient safety implications, so regulators come down hard.
Compliance Insight: Modern facility design must integrate a robust Contamination Control Strategy (CCS) from the outset. This includes thoughtful facility layout (unidirectional personnel and material flows, segregation of sterile areas), installation of barrier technologies (isolators or RABS) to separate operators from critical aseptic processes, and redundant utilities (backup generators, dual HVAC units) to maintain environmental conditions even during outages. Environmental monitoring systems should be designed for continuous data collection (viable and non-viable monitoring) with trending software to quickly detect adverse trends.
4. Quality Systems and Oversight Lapses
Beyond technical issues, FDA inspectors often uncover systemic quality management failures- things like incomplete investigations, lack of management oversight, or poor training/documentation practices. In the last two years, many firms have been cited for inadequate QA oversight and weak quality unit authority.
For example, Sun Pharma’s Dadra warning letter (2024) noted that the site did "not operate an effective quality system" and had inadequate oversight of manufacturing, leading to repeat violations. Similarly, Lupin- another Indian generic giant- received multiple Form 483s across different plants in 2022–23; issues ranged from failure to thoroughly investigate batch failures to neglecting proper documentation of deviations.
FDA classified one Lupin plant’s compliance status as Voluntary Action Indicated (VAI)- meaning objectionable conditions were found- and in a span of nine weeks, Lupin was hit with 483s at four different sites, indicating enterprise-wide quality system gaps.
Compliance Insight: An audit-ready facility isn’t just about equipment and environment- it requires a culture of quality and robust quality systems. Project and validation managers should ensure that Standard Operating Procedures (SOPs) for key processes (deviations, Corrective and Preventive Actions (CAPA), change control, complaint handling, etc.) are in place and actually followed from the moment the plant starts operations. Common 483 citations include "procedures not adequately established or followed" for CAPA and complaint handling, so teams must both write clear procedures and train personnel to consistently execute them.
Annex 1 (2023): New Challenges for Sterile Facility Design
Regulators worldwide are raising the bar for facility design, especially for sterile manufacturing. The EU’s Annex 1 revision (effective 2023) is a prime example of stricter standards that directly impact how facilities must be built or upgraded. Annex 1 emphasizes contamination control, modern technology, and quality risk management in every aspect of sterile production.
Key requirements- like implementing a formal Contamination Control Strategy (CCS), using barrier technology (isolators/RABS), and more rigorous environmental and process monitoring- pose significant design and operational challenges for manufacturers.
Design Pain Points Under Annex 1
Several technical areas have proven difficult:
- Barrier Systems: Installing isolators or RABS has been one of the most challenging Annex 1 requirements due to its heavy impact on facility layouts and workflows. Retrofitting an older cleanroom with isolator technology often requires major construction, HVAC reconfiguration, and retraining of staff.
- Environmental Monitoring (EM): The revised Annex demands more comprehensive EM (including continuous particle monitoring in critical zones) and thorough trend analysis. Companies have struggled to meet these expectations, ensuring continuous, viable monitoring or conducting meaningful trend reviews of microbial data has required new monitoring systems and data analytics tools.
- Cleanroom Classification & Qualification: Annex 1 introduced stricter criteria for cleanroom qualification (e.g., more robust airflow visualization studies and periodic re-qualifications). About 35% of companies in the survey struggled with the tighter cleanroom standards, particularly around airflow pattern tests (smoke studies.
- Cleanroom Classification & Qualification: Annex 1 introduced stricter criteria for cleanroom qualification (e.g., more robust airflow visualization studies and periodic re-qualifications). About 35% of companies in a recent survey struggled with the tighter cleanroom standards, particularly around airflow pattern tests (smoke studies) and meeting new classification specs. This has direct implications for HVAC design and room layout.
- Aseptic Process Simulations (APS): Media fill simulations are under greater scrutiny. Annex 1 expands guidance on handling interruptions, incubation times, and validating isolator-based processes. Many firms struggled to interpret APS requirements correctly and failed to incorporate simulation capacity into equipment design.
- PUPSIT (Pre-Use Post-Sterilization Integrity Testing): Annex 1 mandates PUPSIT for sterilizing filters unless well-justified. However, nearly 40% of companies hadn’t implemented it, citing technical or layout constraints. Failing to perform PUPSIT or justify its omission is now a common inspection trigger.
Regulatory Scrutiny is Real
More than half of recent FDA and MHRA inspections have included a review of Annex 1 implementation- especially CCS, APS, environmental monitoring, and barrier systems. However, differing interpretations by regulators across geographies add further complexity.
Design Strategy
To ensure compliance with Annex 1:
- Conduct a detailed gap assessment against Annex 1 for new and legacy facilities
- Engage cross-functional SMEs- QA, microbiology, process, validation- early in the design phase.
- Adopt technologies Annex 1 favours: automated EM systems, robotics, RABS/isolators.
- Include training zones and media fill capacity in early facility planning.ng
- Treat Annex 1 as a performance blueprint, not just a checklist
When approached proactively, Annex 1 doesn’t just raise the compliance bar- it becomes an opportunity to enhance sterility assurance and operational excellence.
Strengthening CQV: Validation as the First Line of Defence
With the rise of surprise inspections, the FDA is intensifying its focus on Commissioning, Qualification, and Validation (CQV) across all GxP systems. Validation lapses- from unqualified equipment to unvalidated software- are among the top five causes of Form 483s globally.
Key CQV Pitfalls
- Equipment and utility not qualified (IQ/OQ/PQ missing or outdated)
- Lack of PPQ or insufficient process verification post-launch
- Unvalidated computer systems (e.g., MES, LIMS, SCADA)
- No documented change impact assessments
- Incomplete cleaning or analytical method validation
Validation Must Be Lifecycle-Based
Validation is not a one-off activity- it must be continuous. FDA expects manufacturers to:
- Maintain a master validation plan
- Document equipment requalification after changes
- Track utility performance (e.g., water systems, HVAC) with trending data
- Show continued process verification (CPV) post-PPQ
- Ensure 21 CFR Part 11 compliance across all software platforms
- Maintain validation packs that are audit-ready (URS → IQ/OQ/PQ → summary reports)
✅ “If it isn’t documented, it didn’t happen.” – FDA GMP principle
By embedding validation readiness into the project lifecycle, companies not only avoid compliance gaps but build operational trust- internally and externally.
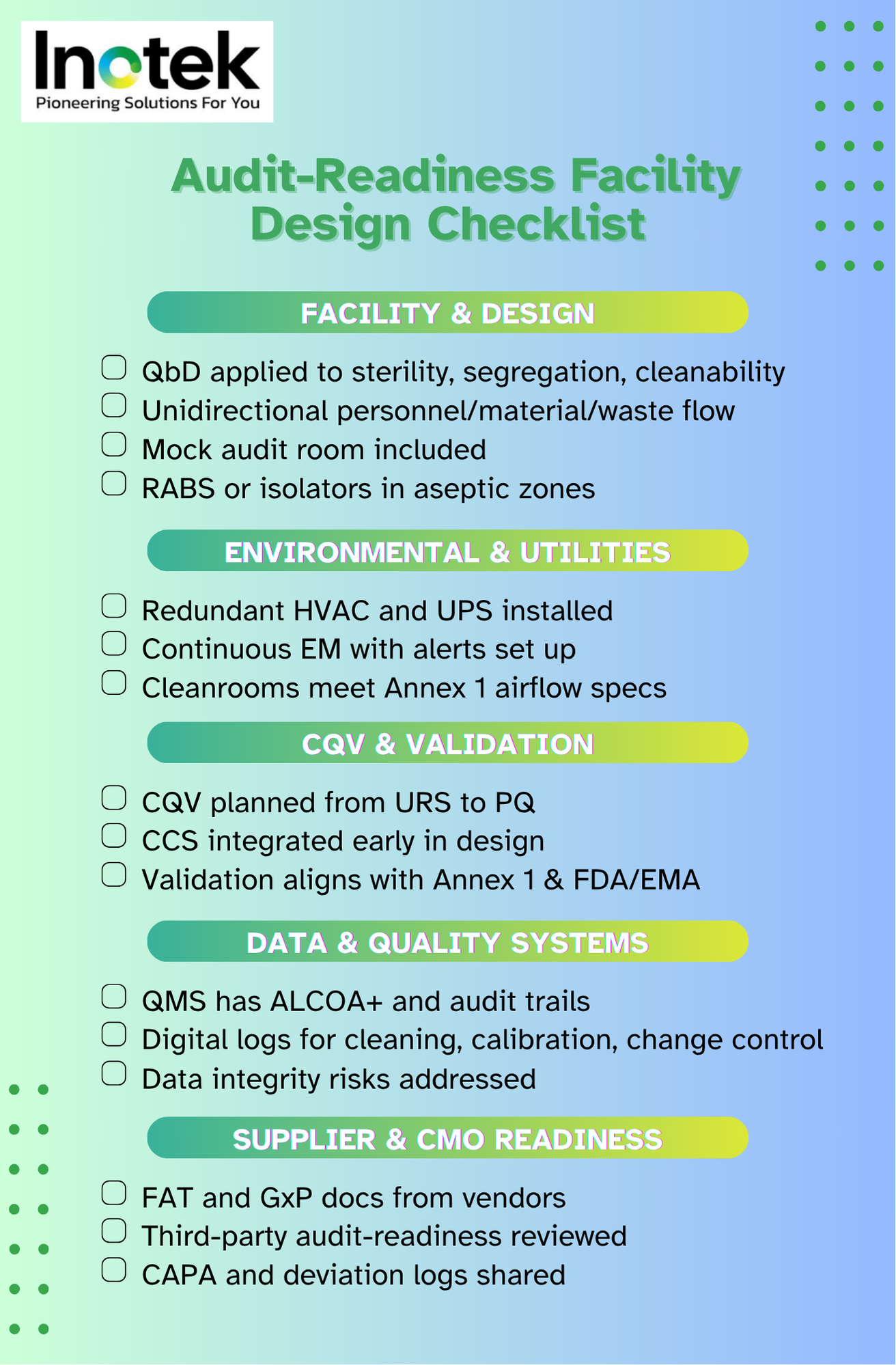
Designing Audit-Ready Facilities: A Structured Playbook
Whether you’re building a greenfield plant or retrofitting a sterile suite, audit readiness starts on the drawing board. The following are key design principles that forward-looking project teams are implementing:
- Quality by Design (QbD):
Prioritise sterility, cleanability, and segregation as Critical Quality Attributes (CQAs). Build layouts and systems with these as foundational elements. - Unidirectional Flow:
Ensure personnel, material, and waste flows never intersect. Use airlocks, interlocks, and clearly separated pathways. - Environmental Monitoring (EM):
Deploy continuous, viable, and non-viable monitoring in critical areas. Integrate with cloud-based dashboards for real-time alerts. - Barrier Technology:
Adopt isolators or Restricted Access Barrier Systems (RABS) for aseptic zones to minimise manual interventions. - Power & HVAC Redundancy:
Install UPS for sensitive systems like incubators and redundant HVAC to protect cleanroom conditions during outages. - Human Factor Design:
Design for compliance: ergonomic gowning spaces, on-wall SOP displays, instructional signage, and digital status boards. - Mock Audit Zones:
Include dedicated “war rooms” for inspections, equipped with document access systems and seating for interviews. - Supplier-Integrated Readiness:
Require FAT, GxP documentation, and design-stage reviews from vendors supplying equipment, skids, or modular systems.
Global Implications for Outsourcing and Supply Chain Integrity
If you’re sourcing APIs or drug products from India or China, your regulatory risk is not outsourced- it’s inherited.
With over 2,000 foreign sites overdue for FDA inspection (as of 2024), many global pharma sponsors are exposed to non-compliance at third-party facilities.
Key Recommendations
- Pre-qualify partners thoroughly: Use GMP site audits, history of FDA 483s, and current remediation status.
- Mandate visibility in quality agreements: Require notification of inspections and Form 483s. Include audit rights and unannounced access clauses.
- Joint quality reviews: Schedule quarterly calls to discuss deviations, CAPAs, EM data, and change control.
- Develop redundancy and inventory buffers: In case of import alerts or compliance holds, ensure product continuity.
- Support partners with tools/training: Many sponsors now offer Annex 1 or data integrity workshops for CMOs.
By approaching audit-readiness as a collaborative goal, sponsors de-risk their supply chain and foster long-term manufacturing resilience.
From Blueprint to Batch Release- Compliance is a Design Decision
Unannounced FDA inspections are not a passing trend- they are the future of GMP enforcement.
To withstand them, pharma companies must reframe how they approach facility design. GMP is not just a layer of SOPs and checklists- it’s an operating philosophy that must be baked into the physical infrastructure.
From robust CQV protocols and Annex 1-ready cleanroom layouts to digital validation systems and empowered QA functions, audit-readiness must be visible in every inch of the plant.
The best time to prepare for a surprise audit is before the facility even opens its doors.
Inotek Delivers Inspection-Ready Projects from Day One
The complexities of audit-ready pharma facility design demand specialised expertise and compliance-focused execution. This is where Inotek steps in as your strategic partner.
We don’t just prepare facilities for inspections; we engineer regulatory resilience and data-driven compliance into every facility we deliver, aligned with global regulatory standards like FDA, EMA, and CDSCO.
Our comprehensive approach includes:
CQV Lifecycle Management: End-to-end Commissioning, Qualification, and Validation (IQ/OQ/PQ/PPQ) to meet global GxP expectations and withstand FDA scrutiny.
Annex 1-Compliant Cleanroom Design: Barrier systems (RABS/Isolators), CCS integration, and airflow zoning to meet EU Annex 1 and ISO 14644 requirements.
Real-Time Data Integrity Systems: ALCOA+-based digital infrastructures with audit trails, time-stamped records, and validated software platforms to eliminate data integrity risks.
Mock Audit & Inspector Access Zones: Strategically designed “war rooms” and documentation hubs to facilitate smoother, faster audits.
CMO & Supplier Qualification Frameworks: Structured protocols for partner audits, FATs, and integrated vendor documentation to reduce third-party compliance risk.
By partnering with Inotek, pharma manufacturers have achieved:
- Faster facility commissioning and audit clearance timelines
- Significant reduction in Form 483 observations and CAPAs
- Higher inspection confidence among regulators and QA teams
While compliance forms the foundation, successful audit-ready facility design must also address growing industry expectations around:
- Supply chain visibility and CMO oversight
- Digital validation systems and Part 11 adherence
- Scalable design for future regulatory updates (e.g., revised Annexes, FDA guidances)
At Inotek, we ensure your facility isn’t just audit-ready- it’s engineered for long-term operational excellence and regulatory trust.
Recognised among the Top 10 Pharma Turnkey Contractors & Project Consultants in 2022 & 2025, Inotek helps pharma leaders design, build, and upgrade facilities that meet the strictest GMP and sustainability standards.
📞 Connect with our experts today or visit www.inotek.co.in to schedule a consultation with Mr. Rohit Ochaney.
Whether you're planning a greenfield facility or optimising an existing setup, Inotek ensures your project is compliant, resilient, and future-proof.
FAQs
What are surprise FDA inspections, and why are Indian pharma plants facing more of them?
Unannounced FDA inspections are audits conducted without prior notice. Since 2023, Indian pharma sites have seen a rise in these inspections due to GMP concerns and long inspection gaps post-COVID.
How can pharma companies in India prepare for a surprise FDA audit?
Indian pharma firms should integrate audit-readiness into facility design, ensure ALCOA+ compliance, validate equipment proactively, and maintain digital documentation for traceability.
What are the top reasons Indian pharma facilities fail FDA inspections?
Common failures include data integrity issues, unqualified equipment, poor contamination control, and missing validation documentation. Legacy facilities are especially at risk.
What does the FDA expect during an unannounced inspection in India?
The FDA expects immediate access to QMS, CCS, validation documents, equipment logs, and SOPs. Delays or incomplete records can result in 483s or import alerts.
How should Indian pharma project teams incorporate Annex 1 into facility design?
Teams must plan CCS early, adopt isolators or RABS, ensure airflow zoning, and meet new environmental monitoring standards to align with Annex 1 and FDA requirements.
Who can help design FDA-compliant pharma facilities in India?
Consultants like Inotek offer end-to-end support- from URS and cleanroom layout to CQV and mock audits- ensuring Indian pharma plants meet FDA, EMA, and CDSCO expectations.




